Removal of Breast Implants alone or with Uplift (mastopexy)
Why do some patients have their breast implants removed?
Most patients will renew their implants, but occasionally some patients decide they want to have them removed and not replaced (explantation).
The breasts after explantation will be smaller, flatter, emptier and the skin will be loose with a lower nipple position. The results look worse if you have had very large implants and you have very thin tissue covering the implants, as when they are removed the breasts will look like empty bags of skin. It may affect your confidence and you must think carefully about how you will feel before having your implants removed.
These are situations where patients have reported a desire to have their implants removed:
-
- Original enlargement was with implants that were too big and the patient now desires being smaller again. As long as this is done soon after breast augmentation breast shape returns quickly. If the implants have been in for years, there will be permanent age related changes and tissue sag. Patients with sag can opt to have a limited breast uplift (mastopexy) at the same time, which will improve nipple position and remove excess skin. This is called a wise pattern dermo-cutaneous mastopexy. If patients want to have the implant capsules removed at the same time this can usually be accommodated and we can aim for total capsulectomy and often employ an en-bloc technique as long as it does not put the patient at excess risk of serious complications.

The above photo is an example of the outcome in a lady who had old 280cc implants removed, and at the same time Mr Turton carried out a wise pattern breast uplift (demo-cutaneous mastopexy). - Alternatively, patients could opt to have a dermo-cutaneous mastopexy done at a later time having initially decided to see if their breast shape returns to something they are comfortable with.
- Breasts that have got gradually bigger as weight has changed since the original augmentation can also sometimes lead to a desire to remove implants. In this situation you might feel better if the implants are removed. As long as you don’t have a lot of sag, this can work well for some patients. Otherwise you can consider the breast uplift as described above to improve shape.
- Problems with breast implants. A number of patients get problems such as chronic pain, recurrent capsular contraction or a chronic seroma. Sometimes removing the implants is the best or safest option. More recently there has been an increase in requests for removal as patients have become fearful of breast implant illness- this is not a medical term, but a wide collection of non-specific symptoms that some women think may occur due to their implants. And other patients with macro-textured implants decide that they want them removed as they worry about breast implant lymphoma- an uncommon cancer associated with textured breast implants (see section on BIA-ALCL)
- With old age or ill-health it may be that breast implants are no longer desired. The ongoing importance of a nice breast shape may decline such that the cost of renewing implants or monitoring them with Magnetic Resonance Imaging (MRI) or ultrasound (USS) scans becomes a factor and it is simpler to have them out.
- Adult women develop various medical conditions as they age and some of these are associated with symptoms. For example, anxiety and depression are prevalent in the population. Non-specific diseases like fibromyalgia and osteoarthritis coexist in the female population. Vitamin D deficiency with the associated non-specific symptoms of fatigue is common. Primary hyperparathyroidism is common in middle age years and causes raised blood calcium levels with a raised parathormone level that commonly goes undetected for years, but the commonest symptoms are headaches, fatigue, apathy, non specific weakness and apathy. Declining oestrogen levels, often fluctuating for a few years, in the 40s or early 50s is often associated with brain fog, low energy, joint stiffness, hair thinning, change in skin quality, hot flushes, anxiety and depression. When periods are still occurring, it can be easy to dismiss it. And there are many other medical problems that are non-specific in nature. When these conditions arise but are not diagnoses in women with breast implants, it can be a problem if the patient is concerned that it is the implant that is causing the problem. There is much misinformation on the internet and it is possible to become consumed with anxiety from social media influences that the implants are to blame. Whilst I urge all medical doctors dealing with these possibilities to be open-minded that the symptoms might be linked it is important rot remember that the evidence for such a link is not there. Suggestions of an association between some autoimmune disorders and implants do exist is some data series and so looking for such a problem should be carried out in the patient with symptoms of concern. This can be investigated with clinical review and blood tests. Most inflammatory or autoimmune disorders have a positive elevation in inflammartory markers or auto-antibody titres. Hence, never dismiss the small number of patients that develop symptoms and become concerned that their implants are making them ill, have ‘Breast Implant Illness’, or that they may have caused an autoimmune disease. Instead, engage with them using your diagnostic skills. Whilst there is no definite scientific evidence for BII, or evidence that removing the implant and the surrounding capsule tissue has any benefit, some patients request en-bloc capsulectomy and removal of implants. As long as the patient has been educated that the limited studies in their scenario has shown that symptoms may not change or only change temporarily, if they still want an explant then it is reasonable to do so. Consent is the key so they are aware of the alternatives, risks, consequences and complications associated with the procedure. For may women going down this route it is simply a matter of getting peace of mind. Sometimes even with the best reassurance in the world from a consultant that the implant is not causing the problem, having been exposed to social media about the ‘potential’ for this is enough to leave them anxious to have the implants removed.


- Original enlargement was with implants that were too big and the patient now desires being smaller again. As long as this is done soon after breast augmentation breast shape returns quickly. If the implants have been in for years, there will be permanent age related changes and tissue sag. Patients with sag can opt to have a limited breast uplift (mastopexy) at the same time, which will improve nipple position and remove excess skin. This is called a wise pattern dermo-cutaneous mastopexy. If patients want to have the implant capsules removed at the same time this can usually be accommodated and we can aim for total capsulectomy and often employ an en-bloc technique as long as it does not put the patient at excess risk of serious complications.
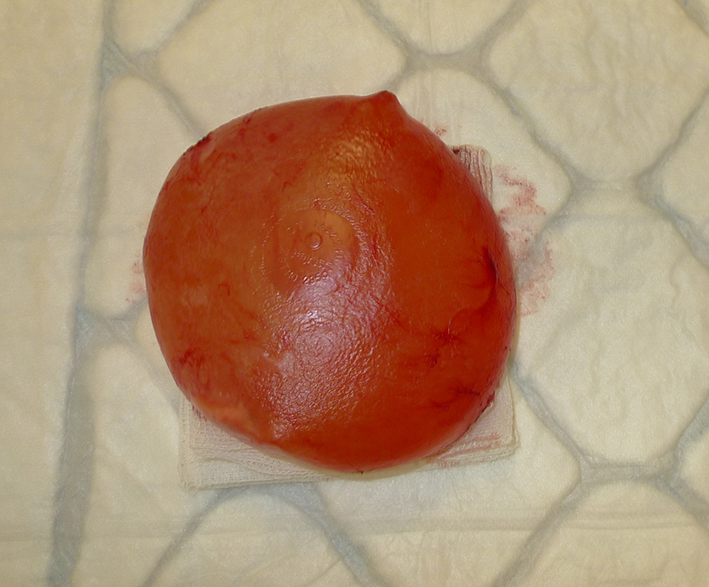
Here is an example of total en-bloc capsulectomy. In the centre photo above, you can see the thin pink/red capsule is still fully intact with the breast implant still inside. Only after the operation has completed will Mr Turton incise to open the capsule. This is done ‘on a separate trolley’ away from the operating area. This enables him to safely remove and inspect the inside of the capsule. In this example (top left photo) you see a very thin almost transparent capsule. There is no abnormal pathology with this, and apart from the fact that it was contracting, it was not an adverse finding. The final part is the inspection of the implant. He makes note of the type of implant, its texturing and whether it was leaking. And then finally to send the capsule tissue to breast histopathology for testing requires further care. Usually this is done with full orientation of the capsule tissue for the pathologist, by placing marking sutures to define the front and back surface, the top bottom and inner and outer edges. That way, if any adverse pathology was to be discovered, it can be linked back to where in the capsule it occurred. Mr Turton works with specific consultant breast pathologists who are experienced with dealing with breast capsules. The histology results are usually ready 10-days after surgery.
In this example, a patient with 30-year old breast implants presented with terrible breast sag over the implants. She also had decided that she no longer wanted the implants and wanted to have capsulectomy too. After assessment we agreed on a combined removal, capsulectomy and full breast uplift.

Breast Sag in a patient with old cosmetic implants
Her results after explantation and caspulectomy and full breast uplift are shown at just over 5-months, with a lovely result.
Risks and Complications of Explantation
The risks of serious complication from explantation are usually quite small. The main problem is the cosmetic impact for patients and that must not be ignored. The operation is usually always carried out under a general anaesthetic. If the implants are being removed due to problems such as capsular contraction or rupture then there may be extra work to do to remove capsule tissue. If total capsulectomy or en-bloc capsulectomy is required, then the surgery always takes longer and is quite painstaking. Removing the capsule in its entirety is occasionally essential in cases related to lymphoma in the capsule (BIA-ALCL). This is called en-bloc capsulectomy. It is always a more complex operation and when the implants are infront of the muscle, some muscle tissue is likely to be removed that is adherent to the capsule. When the implants are sub-pectoral and enbloc capsulectomy is done, the back layer is often densely adherent to the ribs, cartilage, and intercostal muscles. Removal of this back layer can usually still be accomplished. But there always has to be the caveat that if there is a concern that it is too dangerous to remove it in places that there would be some capsule partly left- this might be due to the risk of pneumothorax for example. When a full capsulectomy or en-bloc capsulectomy is done the breast pocket, the space where the old implant used to be, is generally of a far greater diameter than before. The normal boundaries having been lost, mean that even if new implants are to be inserted the position of those implants tends to fall to the edges of the space- so there is a deterioration in the cosmetic result compared to someone who did not have the capsule removed. For this reason, we will sometimes recommend not to remove the capsule when it is safe not to do so. If there is an area of capsule inflammation, Mr Turton would usually remove this for histology testing if there was any reason to do so- this is called partial capsulectomy.
In specific circumstances, generally if patients are old and infirm, the implants can sometimes be removed under local anaesthetic.
With capsulectomy surgery when removing implants there is a slightly higher occurrence of haematoma after surgery, which might mean a return to theatre. A few weeks down the line and we see fluid collecting in the old implants space, which is called a seroma. This is perfectly notional in the weeks that follow after the implant has been removed, but this is usually a short term problem only. After capsulectomy, and in particular total en-bloc capsulectomy the chest area feels very sore and tender.
The biggest problem is of course the cosmetic outcome that you are left with and this may leave some patients desiring additional procedures to improve their breasts. We would always advise that you give yourself plenty of time to adjust before making any decisions on additional surgery. You can wear padded bras, and mask the appearance while your breasts and body adjust. If you have problems adjusting, become excessively focused and you feel this becomes intrusive, it would be important that you seek a specialist clinical psychologist who can help, such as Maggie Bellew, at Spire Hospital Leeds. Otherwise get support from your friends, family and your GP.
Secondary surgical procedures after explantation are limited and expensive. If you have a lot of loose skin and a very low nipple position then a mastopexy will help. It brings the nipple back to the front of the breast and removes the skin that hangs below the crease of the breast. But it will not improve the volume. To improve the volume you might consider a series of lipomodelling operations.
Lipomodelling to improve breast shape after explantation.
Lipomodelling is a technique performed under general anaesthetic. Each procedure gives a small improvement only and is expensive because of the hospital, surgical and anaesthetic costs each time. It costs around £2800-£3000 per session. You therefore must be realistic as to what it can achieve. Think carefully about your expectations and then discuss them with Mr Turton.
Localised deposits of fat usually from the lower back, bottom and outer thighs are removed by gentle liposuction, centrifuged to remove oil and blood and then the pure fat is injected in tiny quantities into the thin layer of residual breast tissue that you have and the muscle behind the breast. Fat is a living tissue and so must be injected into tissue (not the empty space where the implant was). The injection technique is critical to achieve permanent survival of the new cells within the breast. Mr Turton injects the fat as multiple layers of adjacent thin long threads like spaghetti, and only a limited amount of fat can be injected at one operation. The new fat cells will only survive for up to 48-hours without being in direct contact with blood vessels to provide oxygen and nutrition; new blood vessels need to form to supply their longer term needs and this process is strongly inhibited in smokers, which would be a complete contraindication to the procedure.
For every 200cc of fat that is collected, about 100cc will remain after centrifuge treatment for re-injection, and then of this around 50% is reabsorbed or broken down by your body before it develops a blood supply in the tissue and becomes stable. Because only about 100cc can be injected per session, you effectively gain 50cc of volume for every 200cc of liposuction procedure and so you would like need 3 lipomodelling sessions to get a noticeable improvement of just 150cc. When doing this on both breasts, the availability of a harvestable fat source becomes a limiting factor in slim patients.
You must wait 4-months in between each session to allow each fat graft time to be incorporated by the breast, so 3 sessions take a year and the costs will come to around £8500-£9000.
How will I feel after lipomodelling?
The incisions used for lipomodelling are tiny (3-4mm). Most patients are discharged the same day and apart from fairly extensive bruising and tenderness at the site the fat was taken they have minimal problems. You can normally go back to work within a few days with the majority of the bruising and swelling going after a week and rest being minor, resolving slowly over a few months. Care must be taken to prevent infection.
Uncommon risks include contour irregularities under the skin from where the fat was taken. Wearing a tight spandex garment reduces the chances of this. Numbness and pigmentation changes may occur but these should settle after several months. Very rare risks might be unknown with lipomodelling – when the procedure was first introduced around a decade ago, there was a theoretical risk that it could slightly increase the risk of breast cancer. This is probably because it was being injected into breasts after mastectomy or lumpectomy for cancer. Whilst this risk has not translated into any significant risk of cancer in practice one must remember that it is theoretically possible because fat contains some cells known as ‘Adipocyte-derived Regenerative Cells’. These are more like primitive stem cells and although the evidence to date does not suggest a higher cancer risk, good quality long term studies are required to prove this although are unlikely to be undertaken.
How will I know if it has worked?
The process of liposuction is traumatic to the fatty tissue and some of the cells will not survive after they have been suctioned, separated form the blood and oil by being centrifuged and injected back in to your body .
If it is repeated too quickly you will experience hard lumps of dead fat (fat necrosis) and oil cysts will form. Lipomodelling to the breast always causes tiny micro-calcifications to appear on future mammograms which can interfere with assessment for the early changes of breast cancer, lead to extra tests such as biopsies to work out the cause and cause you anxiety.
Organise your consultation with Mr Turton: Specialist Consultation Booking Form


